
For example, HMGB 1 stimulates coagulation cascades by upregulating tissue factor expression and promoting the externalization of phosphatidylserine to the outer surface of the cell membranes. In addition to the effects of NETs, damage-associated molecular patterns including cell-free DNA, histones, and high-mobility group box 1 (HMGB 1) are released into the bloodstream from the damaged or necrotic cells that can activate procoagulant effects (Fig. reported the increased capability of NETs formation of the neutrophils obtained from sepsis-associated DIC. NETs are also known to convert the anticoagulant property of the vascular endothelium to procoagulant. NETs are composed of DNA, histones, and other cytotoxic substances that immobilize and eradicate invading pathogens. The immunothrombus formed by leukocyte-platelet aggregates and fibrin deposition in the vascular lumen is the hallmark of sepsis-associated DIC. Intravital microscopic observation of sepsis models demonstrate the injurious effects of neutrophil adhesion, platelet aggregation, and morphological changes of endothelial cells (Fig. The vascular endothelial cell is the primary target of injury in sepsis-associated DIC from polymorphonuclear neutrophils that are activated, releasing neutrophil extracellular traps (NETs), reactive oxygen species, and other proinflammatory mediators.

are necessary for the success in the development of new therapy. The ideally designed studies that determine to whom, when to start, for how long, and how much, etc. The natural anticoagulants such as antithrombin, protein C, and thrombomodulin are the first candidates that should be examined. Since the fibrinolytic suppression is a result of activated coagulation, we think anticoagulant therapy may be the better choice. However, the appropriate control of fibrinolysis is not easy, and the fibrinolytic approach may not be a good choice. Upon these findings, balancing coagulation and fibrinolysis is expected to provide an opportunity for future therapeutic agent development. Multiple studies have reported the increased level of PAI-1 is a useful marker of poor outcome in sepsis. Perhaps, this fibrinolysis suppression has the purpose of restricting the pathogen spread and tissue healing but leads the unfavorable microcirculatory disturbance.
#Dic lab findings Activator#
Virtually, the thrombotic-type DIC is characterized by the suppressed fibrinolysis, and plasminogen activator inhibitor-1 (PAI-1) produced by endothelial cells contributes to the fibrinolysis suppression. The suppression of fibrinolysis, often referred to as fibrinolytic shutdown, plays a major role in accelerating the prothrombotic condition. Thrombin has a multitude of effects beyond clot formation that include endothelium activation by binding to protease activated receptor 1 (PAR-1) expressed on the endothelial surface and platelets to amplify inflammation. Among the coagulation factors, thrombin is considered to be the central factor in the pathogenesis of sepsis-associated DIC. Furthermore, the extracellular vesicles released from various cells also express the tissue factor in sepsis-associated DIC. The mechanisms of the activation in coagulation and inhibition of fibrinolysis are multifactorial, but the principal initiator of the coagulation cascades is considered to be tissue factor that is expressed on macrophages and other cells, including neutrophils and endothelial cells. Currently, the accepted concept is that systemic activation of coagulation and the suppressed fibrinolytic pathways are the major facilitators of multiorgan dysfunction and death.

Recently, the importance of early coagulopathy detection before patients decompensate is important for sepsis management.
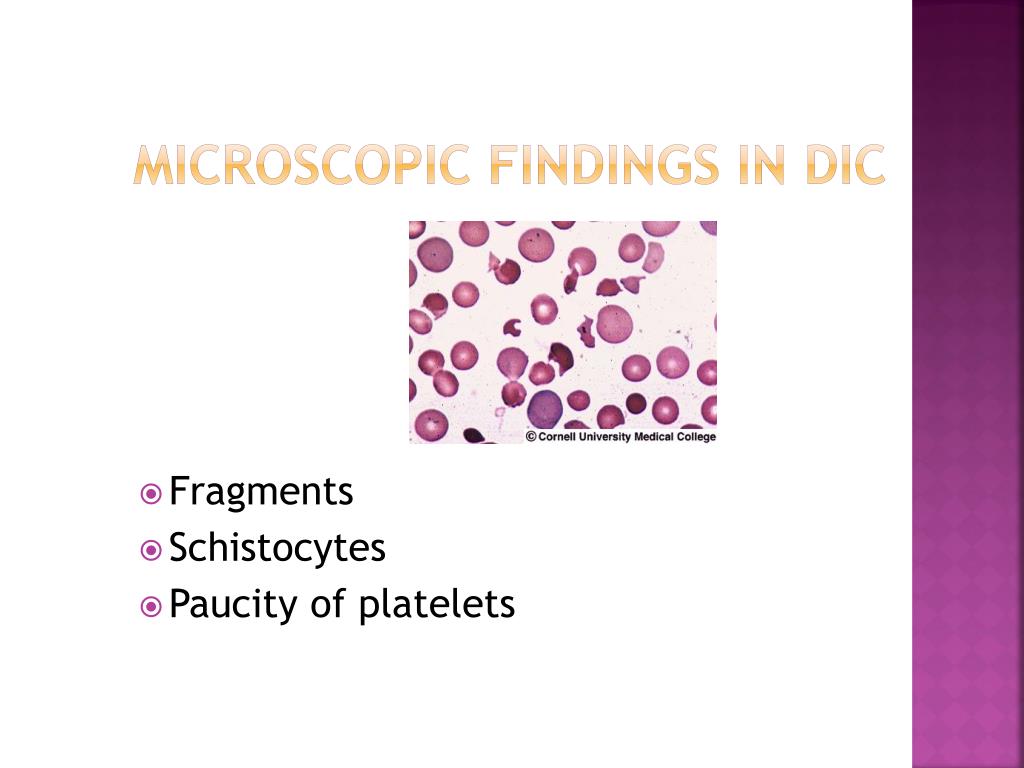
As a result, coagulopathy and its advanced stage of DIC are often considered as the hemostatic disorder. This definition reminds us that “systemic activation in coagulation” is the critical aspect of DIC, however, since it was not possible to construct diagnostic criteria that depict “systemic activation in coagulation” with the conventional coagulation biomarkers, the ISTH published overt DIC diagnostic criteria to better define a consumptive coagulopathy. It can originate from and cause damage to the microvasculature, which, if sufficiently severe, can produce organ dysfunction”. The fundamental concept of DIC was defined as “an acquired syndrome characterized by the intravascular activation of coagulation with loss of localization arising from different causes. Systemic activation in coagulation and fibrinolysis suppression


 0 kommentar(er)
0 kommentar(er)
